Don’t let that scary word “nihilism” keep you from watching this video, which offers optimistic wisdom on dealing with your existential anxiety: that is, fear of death and need for meaning in your life.
Here’s what therapy can do for you
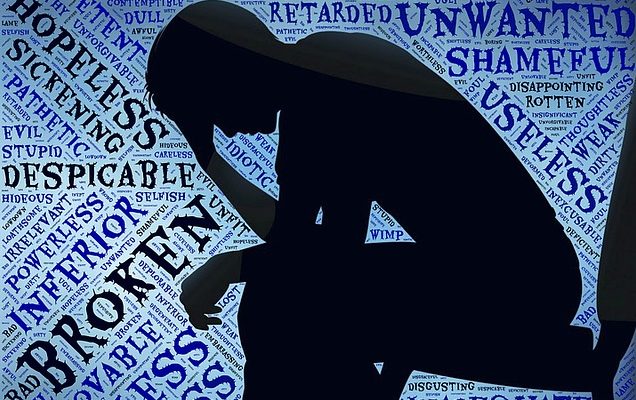
Depression: Is it a Disease or State of Mind?
Depression is one of the most common mental disorders. According to National Institute of Mental Health, 6.7% of all US adults aged 18 or over (about 15.7 million people) suffered at least one major depressive episode in the past year. Many more people have episodes that don’t fit the DSM-5 definition of Major Depressive Disorder, but are still painful and debilitating.
CC0 public domain image from pixabay.com
Disease or state of mind?
People commonly ask: is depression a “disease,” or simply a “state of mind.” This is more than an academic question: our understanding of the roots of the disorder profoundly effects how we treat it. Identifying it as a disease means we’re using a medical model to understand what’s happening. We know that sometimes, your brain physically malfunctions. If it’s a medical problem, then we need a medical solution.
But the causes of human thinking, feeling and behavior are incredibly complex and cannot be reduced to simple biochemical processes. We clearly must take a more nuanced approach to treating mental disorders than we do with something like a virus.
Depression is a difficult, multi-faceted condition, that affects people in different ways. It’s much more than just “feeling sad”: the DSM-5 lists nine different symptoms of major depression, from insomnia to suicidal thoughts, that you might experience. Few suffer from all of them, and many experience only a few. And our treatment of depression varies greatly, depending on the sufferer. Sometimes, it simply goes away on its own. Other times, we can use medication to restore a client to his or her normal outlook on life. (Of course, not everyone responds to the same medication in the same way, so that’s another variable.) And for others, therapy — short-term, long-term, or somewhere in between — works. Finally, many respond best to a combination of therapies.
Help for depression is available
The bottom line, it seems, is that, like most mental illness, our understanding of depression, and how to best treat it, is frustratingly inexact. There’s even evidence that which type of treatment works best depends on the roots of the depression. The most important lesson, however, is simply that regardless of how you define it, depression can be treated successfully. You can get help to reduce your suffering.
What is “Sobriety,” Anyway?
Over on HuffPost, @jasoncherkis has written a brilliant and provocative look at the state of opioid addiction treatment here in the U.S. It’s long, but well worth your time, especially if someone you care about is struggling with addiction and sobriety. The article outlines the inadequacies of our current approach to treating addiction, and hammers home the point that the consequence of failed treatment is often death. It asks whether our moralistic thinking about addiction gives a punitive cast to our treatment choices. And it cites modern medical science to suggest that addiction is at least in part the result of a malfunctioning brain (in the same way diabetes results from a malfunctioning pancreas), and wonders what’s wrong with using medication to repair that malfunction.
But for me, the most interesting question this article raises is: What does it mean to be sober? Surprisingly, a quick Google search, including a visit to the Big Book, reveals that there does not appear to be any agreed-upon definition of “sobriety” among 12-step and other recovery programs! (Here’s a definition that, paradoxically, emphasizes the many possible definitions.) Given that sobriety is the central focus, indeed the goal, of these programs, this seems odd. Some of the definitions my search uncovered include:
- Being free of all intoxicants (which, as you’ll know if you’ve ever attended a 12-step meeting, apparently don’t include coffee and cigarettes).
- “Not being intoxicated,” which is not the same as not consuming intoxicants.
- Living a certain kind of life: responsible, ethical, and with healthy strategies for coping with stress.
I’m sure there are more. The definition is important: how you think of sobriety dictates how you achieve it. This becomes obvious when you consider buprenorphine: the article cites several instances in which people are excluded from treatment because their use of buprenorphine means they aren’t sober. But buprenorphine is designed to suppress cravings and prevent withdrawal symptoms without providing the intoxicating effects of heroin; in other words, when used correctly, it is not an intoxicant. So how is using it breaking sobriety, unless you define sobriety as being free of all psychoactive substances, even life-saving, prescribed medications like antidepressants or anti-psychotics?
This discussion isn’t abstract, but goes directly to the question of how we help people who are suffering from addiction be healthy, happy and productive. Cherkis’ story details over and over again that our current model of addiction recovery works well as long as you are in a controlled setting like a sober living center. But the story makes a strong case that hard-won sobriety often cannot survive in the outside world. Indeed, often the addict cannot survive in the outside world. There’s something worrisome about using a model that insists on limiting itself to using self-discipline, introspection, social support, and spiritual appeals, when so often that model fails, and at times catastrophically. Sure, it’s better when addicts are able to be sober without relying on medications. But it seems misguided to pursue that ideal when the price for failure can literally be death, and there’s an alternative that, while less “pure,” preserves life.
Psychedelics and Mental Health
This New Yorker article is a long and fascinating exploration of recent experiments in the use of psychedelics to treat various mental illnesses and conditions, including addiction, depression, obsessive-compulsive disorder, anxiety, and even existential dread and despair. It raises more questions than it answers (your psychiatrist or doctor isn’t likely to be prescribing you a psilocybin trip anytime soon) but it reinforces the idea that the human mind is astonishingly complex and our understanding of how it works remarkably thin. What we don’t know dwarfs what we do know, and that includes how to treat mental disorders. For me, the key message of this article is this: Psychedelics may not become a standard treatment tool anytime soon, but in the struggle to reduce human suffering, we shouldn’t rule anything out.
A (not so-) Surprising Path to Authenticity
An old friend of mine recently told me that she would soon be taking classes to learn to teach English as a second language. The school she’ll be attending, she casually revealed, is in Mexico.
“You’re leaving the country?” I asked in surprise. Yes, she said. After she completes the training, she intends to spend at least another six months teaching somewhere outside the U.S. She explained that she had always wanted to live overseas, and even though most people who become expatriates do it when they’re young, she felt this was her opportunity, so she’s going.
I was stunned. I knew she was dissatisfied with her life, including the fact that the reward for her decades of professionalism and commitment to her career had been sudden unemployment. But it hadn’t occurred to me that she would suddenly pull up stakes and light out for the territories. My first thought: “She’s a middle-aged woman with a house and friends and family… how can she just leave?”
But then I thought about it some more, and the plan began to sound reasonable, appropriate, sane. She has always had wanderlust and has never been afraid to go to new and exotic places. And although she was successful and expert in her work in the corporate world, she never liked it much (and at times, seemed to positively hate it). It paid her bills, certainly, but she never seemed comfortable, and seemed continually frustrated by the lack of respect she received as well as the ever-decreasing meaning she took from the work itself.
In other words, what I saw as surprising is actually perfectly rational, understandable, and healthy. To use a bit of therapist jargon, her plan reflects authenticity: she’s bringing her life in line with her sense of self. For years, she has played a role – professional, corporate employee, cubicle dweller – and played it pretty successfully, earning decent money and status. But she was wearing a mask, doing what she was supposed to do rather than what satisfied her soul. She was living inauthentically.
It’s difficult, and perhaps impossible, to be happy while living inauthentically. It leaves you constantly battling your “true” self, the real you that we often hesitate to reveal to others (or admit exists even to ourselves). You’re encountering that authentic self every time that small, quiet internal voice reminds you that things aren’t quite right. When we can’t or won’t listen to that reminder, our inner lives become a battleground between what we “should do” and what we want to do. Living with that battle is, at best, tiresome – think of all the energy you’re using just trying to convince yourself that you’re doing the right thing – and at worst, leads to anxiety and depression.
We have many reasons for not living authentically. We tell ourselves, “It would be irresponsible,” or “They [parents, friends, Twitter…] would think I was being foolish,” or “It’s too hard risky, scary, etc.].” The common thread is that we choose to live in a way that feels uncomfortable because we think that we are supposed to.
The truth is, sometimes we do have to do what we’re supposed to. We may have to work a job we hate, that feels completely wrong for us, because we need to support a family. But many (most?) of us can’t keep denying that inner voice forever. At some point, our happiness depends on finding a way to live authentically. Otherwise, we’re unhappy, conflicted, anxious, depressed.
Back to my friend: after many years, she had had enough of living inauthentically. She has arrived at the point where her need for authenticity trumps all the rationalizations and fears that trapped her her in a less-than-fulfilling life. And so, she’s off on an adventure, which I’m guessing will come with its own share of stresses and frustrations. But I’m sure that, any difficulties aside, it will feel exciting, and life-affirming, and authentic. She deserves nothing less.
Sharing Secrets
Post Secret describes itself as “an ongoing community art project where people mail in their secrets anonymously on one side of a postcard.” That’s a deceptively simple description of a profound project: Post Secret gives us all a safe opportunity to share our secrets – whether deep and dark or funny and light. The secrets include confessions of love (often unrequited), infidelity (actual as well as contemplated), minor and not-so-minor moral or ethical violations, descriptions of unusual superstitions or beliefs, and (far too often) self-destructive or suicidal thoughts. When browsing the secrets, I am often moved to tears, and feel privileged that people are willing to share with me.
The benefits of anonymous sharing for the secret-sharer are obvious: most of us have experienced the powerful relief that comes from revealing a long-held secret. But I think the real secret of Post Secret is the benefit it offers the reader: being witness to other people’s silent suffering engages our empathy and humanity to move and educate us. And if you browse long enough, you may make a liberating discovery: “Other people have secrets just like mine!” You aren’t “weird” or strange, just human, and maybe don’t need to feel the guilt and shame that’s been haunting you. So take a moment to visit the site and browse the secrets. It’s a beautiful, healing experience.